MALS: Understanding, Diagnosing, and Treating a Rare Condition
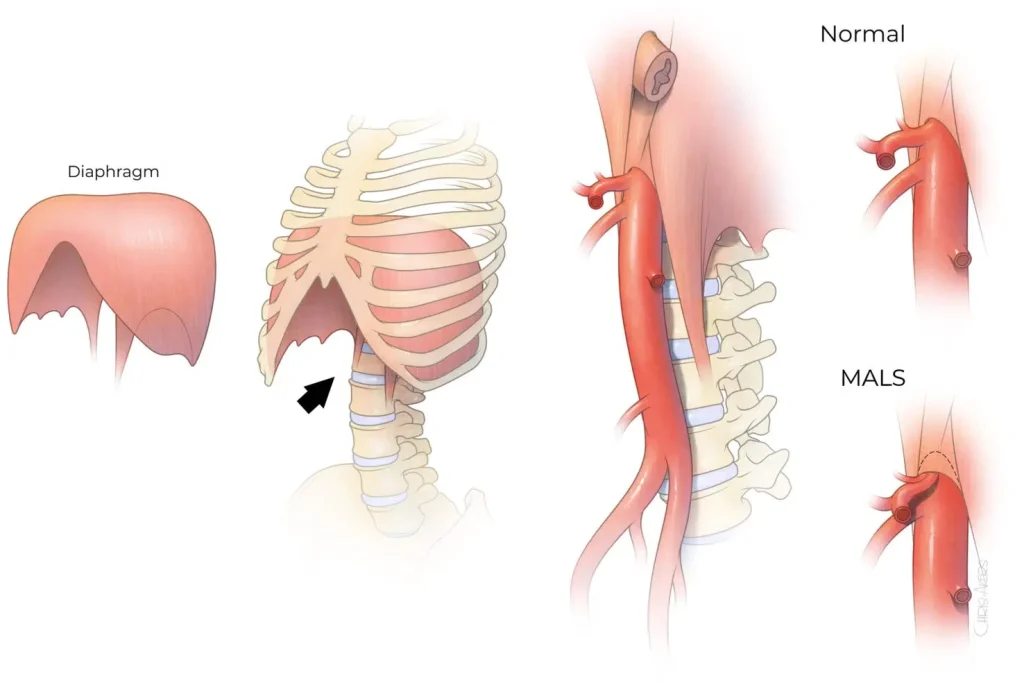
Median Arcuate Ligament Syndrome (MALS) is a rare but potentially debilitating condition caused by the compression of the celiac artery by the median arcuate ligament. This anatomical abnormality can restrict blood flow through the celiac artery to major abdominal organs, leading to symptoms that are often mistaken for other gastrointestinal disorders. Patients with MALS commonly experience epigastric pain, chronic abdominal pain, nausea, vomiting, and unintentional weight loss. Due to its rarity and overlapping symptoms with conditions like irritable bowel syndrome (IBS) and appendicitis, MALS can be challenging to diagnose. However, early detection and appropriate treatment can significantly improve the quality of life for those affected. In addition to his expertise in MALS, Dr. Tierney is also highly regarded as a superior mesenteric artery syndrome specialist.
Symptoms of MALS
MALS symptoms vary but often include sharp upper abdominal pain, especially after eating or exercising. Nausea, vomiting, and unintentional weight loss are common, as patients may eat less to avoid discomfort. Other possible symptoms include bloating, diarrhea, and fatigue, making diagnosis challenging since these overlap with other conditions. Commonly reported symptoms include:
- Upper Abdominal Pain: Often described as a sharp or burning pain, especially after eating or exercising.
- Nausea and Vomiting: These symptoms can occur frequently and may worsen after meals.
- Unintentional Weight Loss: Many patients lose weight due to reduced food intake caused by pain and discomfort.
- Other Symptoms: Some patients may also experience bloating, diarrhea, or fatigue.
Recognizing this spectrum of symptoms is crucial for early diagnosis and treatment. Since the severity and type of symptoms can vary widely, a comprehensive evaluation by a medical professional is essential to determine whether MALS is the underlying cause. Early intervention can help prevent further complications and provide relief from debilitating symptoms.
Diagnostic Process for MALS
Computed Tomography Angiography (CTA)
This is the most recommended imaging technique for detecting vascular compression and assessing the celiac artery's condition.
Doppler Ultrasound and Duplex Ultrasound
Provides real-time assessment of blood flow and can help visualize the artery and celiac axis compression.
Magnetic Resonance Angiography (MRA)
Often used for children or young adults to avoid exposure to ionizing radiation.
Angiogram
This procedure may be used if initial imaging tests are inconclusive, allowing for direct visualization of the blood vessels and confirming the presence of arterial compression.
Treatment Options for MALS
Conservative Management
Lifestyle changes include eating smaller, more frequent meals and avoiding foods that trigger symptoms. Gastric emptying tests may help establish the relationship between MALS and delayed gastric emptying. Medications may be prescribed to manage pain or other symptoms related to gastrointestinal function, such as those associated with gastrointestinal symptoms.
Minimally Invasive Surgery
Surgical intervention may be necessary if conservative treatments are ineffective. Laparoscopic surgery for MALS, such as the laparoscopic release of the median arcuate ligament, is a common approach. This minimally invasive procedure typically results in a shorter recovery time, less pain, and a lower risk of complications than traditional open surgery. Endovascular options may also be considered in some instances.
Multidisciplinary Approach
Effective management of MALS often involves a team of specialists, including gastroenterologists, vascular surgeons, and pain management experts, working together to provide comprehensive and personalized care. This collaborative approach is critical for the management of median arcuate ligament syndrome and the surgical treatment of MALS.
Causes and Risk Factors

The primary cause of MALS is the anatomical compression of the celiac artery by the median arcuate ligament. This fibrous band usually sits above the artery but can sometimes position itself lower than usual, pressing against the artery and surrounding nerves, such as the celiac plexus and celiac ganglion. Several factors can increase the risk of developing MALS, including:
- Rapid Weight Loss: Loss of the protective fat pad surrounding the artery can increase the likelihood of compression.
- Anatomical Variations: Individuals with specific anatomical configurations, like the median arcuate ligament muscle and fibers, are more prone to MALS.
- Demographics: MALS most commonly affects women, particularly those between the ages of 20 and 40. Conditions like Dunbar Syndrome may also be associated with MALS.
At our clinic, Dr. Joshua Tierney brings his extensive expertise in minimally invasive and vascular surgery to the forefront of MALS treatment. With a patient-centered approach, Dr. Tierney specializes in advanced techniques like the laparoscopic release of the median arcuate ligament, providing effective relief for patients suffering from this rare condition. By combining innovative surgical methods with a compassionate understanding of each patient’s unique needs, Dr. Tierney and our team deliver comprehensive care to achieve the best possible outcomes. Dr. Joshua Tierney is recognized as one of the best MALS surgeons, offering advanced, minimally invasive techniques for MALS treatment.
Before surgery
Before undergoing surgery for MALS, the preoperative process generally involves the following steps:
- Comprehensive evaluation, including medical history and imaging studies.
- Discussion of surgery’s risks and benefits.
- Dietary guidelines and medication adjustments leading up to surgery.
- Preoperative instructions provided by Dr. Tierney.
- Possible trial of lifestyle modifications or medications before surgery.
After surgery
The type of surgical procedure you undergo will determine the post-operative care required. Generally, post-surgery care involves:
- Significant reduction in symptoms such as abdominal pain, nausea, and weight loss.
- Quick recovery with most patients resuming activities within weeks.
- Pain management, follow-up imaging, and dietary recommendations for healing.
- Continuous support from Dr. Tierney’s team during recovery.
- Favorable long-term outcomes with lasting symptom relief for many patients.